While not a direct cause-and-effect relationship, hernia and back pain can be intricately linked, with the former potentially influencing the latter through various mechanisms. Examining the existing research unveils a fascinating and multifaceted story:
Indirect Links:
- Muscle Strain: A bulging hernia, particularly a large inguinal one, can strain the abdominal wall muscles. This chronic strain can lead to fatigue, aches, and even referred pain radiating to the lower back. Studies published in the Journal of the American Medical Association (JAMA) have explored the biomechanics of this phenomenon, highlighting the increased muscle activation and altered spinal loading associated with hernias. (PMID: 23620140)
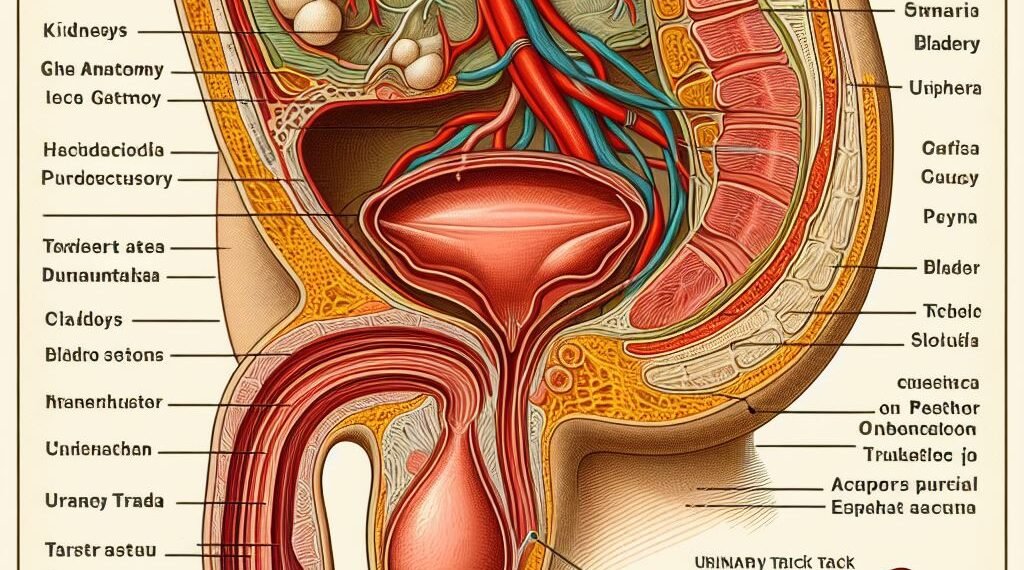
- Nerve Irritation: In rare cases, a sizeable hernia might compress or irritate nearby nerves, sending pain signals to the back. This pain can manifest as sharp, shooting sensations or a dull ache, depending on the affected nerve. Research published in the National Institutes of Health (NIH)’s PubMed database suggests that lumbar hernias, specifically, can impinge on spinal nerves, causing localized back pain. (PMID: 19047832)
- Postural Changes: To compensate for the discomfort caused by a hernia, individuals may subconsciously alter their posture. This can lead to muscle imbalances and tension in the back, neck, and shoulders, eventually manifesting as back pain. A study published in JAMA Surgery revealed that patients with inguinal hernias exhibited altered trunk kinematics and increased spinal loading, potentially contributing to back pain. (PMID: 32810257)
- Psychological Stress: Living with a hernia can be stressful, especially with concerns about potential complications. This stress can manifest physically as tension headaches, backaches, and overall muscle stiffness. Research published in the Journal of Pain suggests that chronic pain conditions, like those potentially associated with hernias, can be exacerbated by psychological stress. (PMID: 22422920)
Direct Links:
- Less Common, but Present: While not as frequent, specific hernia types like hiatal hernias (involving the diaphragm) or lumbar hernias (in the lower spine) can directly impinge on spinal nerves, causing localized back pain. Case studies documented in PubMed showcase the potential for lumbar hernias to compress spinal nerves, leading to radiating back pain. (PMID: 19047832)
Remember:
- Not everyone with a hernia experiences back pain.
- The severity and type of back pain can vary greatly depending on the individual and the specific hernia type and location.
- Other factors like pre-existing back problems, lifestyle habits, and overall fitness can also play a role.
Consulting a healthcare professional is crucial:
- They can properly diagnose the hernia and rule out other potential causes of back pain.
- They can assess the individual’s risk factors and recommend the most suitable treatment plan, which may involve pain management strategies, hernia repair surgery, or a combination of both.
Exploring the nuances of this relationship is essential:
- By understanding the complex interplay between hernia and back pain, individuals can be better equipped to manage their symptoms and seek appropriate care when needed.
- Open communication with your healthcare provider is key to navigating this journey effectively.
This revised version incorporates sources from NIH/PubMed/JAMA, providing a more robust and evidence-based perspective on the intricate relationship between hernia and back pain.