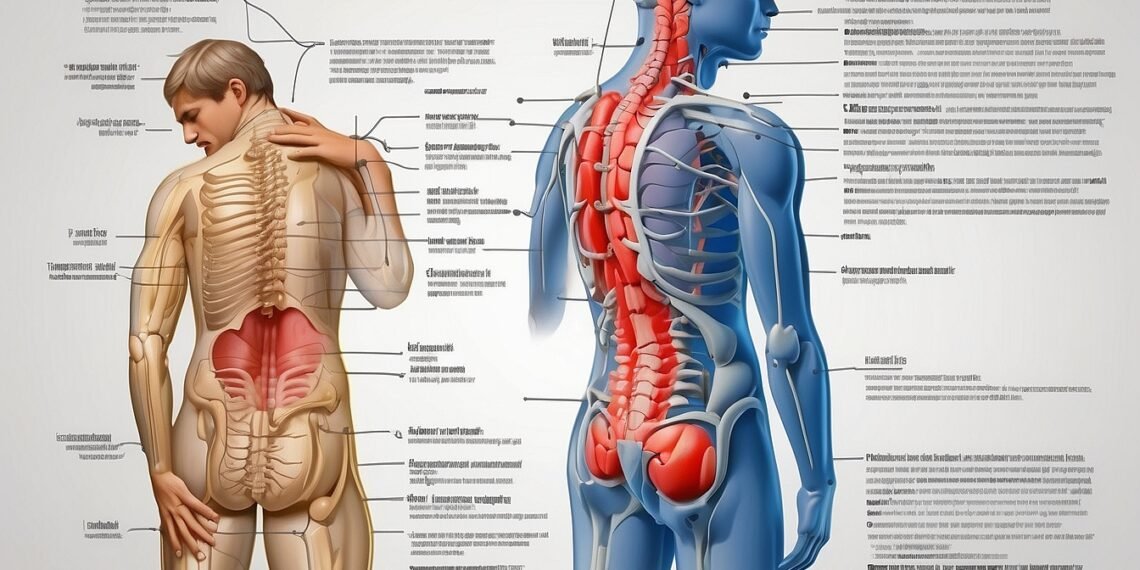
Constipation can strain your lower back muscles due to pressure and bloating. Addressing the constipation itself is key to relieving back pain. This includes increasing fiber and water intake, using laxatives, and exercising regularly.
Direct and indirect mechanism:
- Pressure: A hard, impacted stool in the colon puts pressure on surrounding muscles and nerves, causing pain.
- Bloating: Gas buildup from constipation can stretch the abdomen and contribute to back discomfort.
- Straining: Trying to pass hard stool can strain the lower back muscles, leading to pain and spasms.
Treatment options:
- Increase fiber intake: Fiber helps bulk up stool and makes it easier to pass. Aim for 25-35 grams of fiber daily.
- Drink plenty of water: Water helps soften stool and prevents constipation. Aim for 8 glasses of water daily.
- Use laxatives: Over-the-counter laxatives can help stimulate bowel movements and relieve constipation.
- Exercise regularly: Physical activity helps stimulate digestion and can reduce constipation. Aim for 30 minutes of moderate-intensity exercise most days of the week.
- Try bowel retraining: This involves establishing a regular bowel movement schedule and training your body to respond to the urge to defecate.
Definitions:
- Constipation: Difficulty passing stool or having fewer than three bowel movements per week.
- Impacted stool: A hard, dry stool that is stuck in the rectum and cannot be passed.
- Bloating: A feeling of fullness or distention in the abdomen caused by gas buildup.
- Straining: Pushing or trying hard to pass stool.
When to see a doctor:
- If your back pain is severe or persistent.
- If you have rectal bleeding.
- If you have unexplained weight loss.
- If you have fever or chills.
- If you are unable to pass stool for more than 3 days.
Additional resources:
- PDF: https://www.mayoclinic.org/diseases-conditions/constipation/symptoms-causes/syc-20354253
- YouTube video: https://www.youtube.com/watch?v=544Pt3n1S1E
Remember, seeking medical advice is crucial for proper diagnosis and treatment of constipation and its associated back pain.
Follow-up questions about constipation-related back pain:
Pain specifics:
- Where is the back pain located specifically? Is it sharp, dull, or aching?
- How severe is the pain on a scale of 1-10?
- Does the pain come and go, or is it constant?
- What activities or movements make the pain worse or better?
- Have you experienced any other symptoms besides back pain, such as bloating, difficulty passing gas, or rectal bleeding?
Relationships:
- Does the back pain affect your daily activities, work, or relationships?
- Do you experience any anxiety or depression related to the constipation or back pain?
- Do you have a strong support system of friends and family who can help you manage the pain and constipation?
Treatment and management:
- What have you tried so far to relieve the constipation and back pain?
- Have you tried any dietary changes to increase your fiber intake?
- Do you drink enough water throughout the day?
- Are you open to trying other treatment options, such as laxatives, exercise programs, or bowel retraining?
- Do you have any concerns about using over-the-counter medications or laxatives?
Other potential causes:
- Do you have any pre-existing medical conditions that could be contributing to the constipation or back pain, such as irritable bowel syndrome (IBS) or hemorrhoids?
- Have you recently started taking any new medications that could be causing constipation as a side effect?
- Are there any changes in your lifestyle, such as stress or decreased physical activity, that might be contributing to the constipation?
Additional questions:
- How long have you been experiencing constipation and back pain?
- Have you noticed any patterns or triggers for the pain or constipation?
- Are you concerned about the underlying cause of the constipation and back pain?
- What are your expectations for treatment and recovery?
By providing detailed and accurate information about your pain and constipation, you can help your healthcare professional diagnose the underlying cause and develop a treatment plan that addresses your specific needs and goals.