TOC
- 1 What is deep vein thrombosis?
- 2 Treatment and Prevention Methods for deep vein thrombosis
- 3 Buy compression stockings for DVT
- 4 Purchase blood thinning medications
- 5 Pros and cons of DVT surgery
- 6 DVT vs. pulmonary embolism
- 7 How to prevent DVT during long flights
- 8 Home Remedies for DVT
- 9 DVT during pregnancy
- 10 Resources
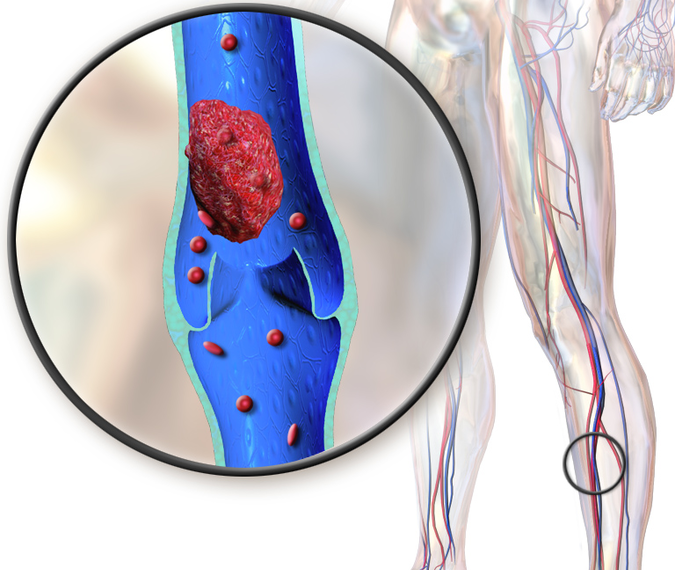
What is deep vein thrombosis?
Deep vein thrombosis (DVT) is a serious medical condition where a blood clot forms within a deep vein, most commonly in the legs. While sometimes asymptomatic, DVT can cause significant pain, swelling, and discoloration in the affected limb. More importantly, it poses a life-threatening risk if the clot breaks loose and travels to the lungs, a condition known as pulmonary embolism (PE).
The Insidious Clot:
Blood clots typically form when an imbalance occurs in the delicate interplay between pro-clotting and anti-clotting factors in the bloodstream. This imbalance can be triggered by various factors, including:
- Venous stasis: Prolonged periods of immobility, such as during long-distance travel or hospitalization, can slow blood flow in the legs, increasing the risk of clot formation.
- Hypercoagulability: Certain medical conditions like cancer, inherited clotting disorders, and pregnancy can make the blood more prone to clotting.
- Endothelial injury: Damage to the inner lining of veins, caused by surgery, trauma, or chronic inflammation, can provide a nidus for clot formation.
Symptoms of deep vein thrombosis
DVT presentation can be a spectrum, with some individuals exhibiting no outward signs at all. This insidious nature underscores the importance of maintaining vigilance, particularly for those at high risk. However, when symptoms do arise, they often involve the affected limb and can include:
- Pain: A persistent, aching pain, often localized to the calf or thigh, is a common symptom. The pain may worsen with activity or standing for prolonged periods.
- Swelling: Unilateral leg swelling, particularly in the calf or ankle, is another characteristic feature. The affected limb may appear visibly larger than the unaffected one.
- Warmth: The skin over the affected area may feel warm to the touch compared to the other leg.
- Tenderness: Pressing on the calf or other areas along the affected vein may elicit tenderness or discomfort.
- Redness: In severe cases, the skin may become discolored, ranging from a faint pink to a deep red.
- Homans’ sign: This test involves passively dorsiflexing the foot (bending the ankle upwards). Pain in the calf or behind the knee when performing this maneuver can be indicative of DVT.
Beyond the Limb:
While the majority of DVT symptoms localize to the affected leg, some individuals may experience more systemic signs, including:
- Fever: Although not a specific symptom, a low-grade fever can sometimes accompany DVT.
- Shortness of breath: This can occur if the clot breaks loose and travels to the lungs, causing PE.
- Rapid heart rate: PE can also trigger an increase in heart rate.
Causes of DVT
- Venous stasis: Reduced blood flow, often due to prolonged immobilization, surgery, or medical conditions like congestive heart failure, creates an environment conducive to clot formation. Endothelial cells lining the veins become exposed to stagnant blood, triggering pro-coagulant signals and impairing fibrinolysis, the natural breakdown of clots.
- Endothelial injury: Damage to the inner lining of veins, caused by trauma, surgery, catheters, or chronic inflammatory conditions, exposes the pro-coagulant collagen subendothelium, initiating the clotting cascade. Additionally, injured endothelial cells release pro-coagulant factors and suppress antithrombotic pathways, further promoting clot formation.
- Hypercoagulability: Inherited or acquired conditions can alter the delicate balance between pro-coagulant and anti-coagulant factors, tipping the scales towards clot formation. Examples include factor V Leiden mutation, protein C deficiency, antiphospholipid syndrome, and malignancies.
- Genetic predisposition: Beyond specific inherited thrombophilia, susceptibility to DVT likely involves complex interactions between numerous genetic variants and environmental factors. Genome-wide association studies are identifying novel genetic loci associated with DVT risk, paving the way for personalized risk assessment and prevention strategies.
- Inflammation: Chronic inflammatory conditions like inflammatory bowel disease and rheumatoid arthritis are increasingly recognized as independent risk factors for DVT. Inflammatory mediators have been shown to activate the clotting cascade, promote endothelial dysfunction, and impair fibrinolysis.
- Microbiome dysbiosis: Recent research suggests an intriguing link between gut microbiota composition and DVT risk. Alterations in the gut microbiome may influence thrombogenicity through various mechanisms, potentially opening doors for novel preventive or therapeutic approaches.
- Environmental factors: Lifestyle factors like smoking, obesity, and air travel also contribute to DVT risk. Smoking damages the endothelium, obesity impairs venous return, and long-distance travel leads to prolonged leg immobility. Understanding these environmental triggers is crucial for lifestyle modifications and targeted prevention strategies.
Treatment and Prevention Methods for deep vein thrombosis
Anticoagulants, aptly named, stand as the cornerstone of DVT treatment. These medications aim to impede clot growth and prevent further thrombus formation, safeguarding against PE. The anticoagulant arsenal boasts several key players:
- Heparin: This fast-acting injectable medication comes in unfractionated and low-molecular-weight heparin (LMWH) forms. LMWH, with its predictable dosing and lower bleeding risk, often takes center stage.
- Warfarin: This oral medication, a vitamin K antagonist, requires close monitoring through INR (international normalized ratio) blood tests to ensure proper blood thinning.
Beyond the Blood Thinners:
While anticoagulants reign supreme, other treatment methods play crucial roles in specific scenarios:
- Thrombolysis and Thrombectomy: For extensive clots or those posing imminent PE risk, clot-busting medications (thrombolytics) or clot-removal procedures (thrombectomy) might be employed.
- Inferior Vena Cava Filters: In specific cases, like recurrent DVT despite anticoagulation or contraindications to anticoagulants, these filters implanted in the major vein leading to the lungs can trap clots before they reach the lungs.
DVT prevention methods
Combating DVT requires a multi-pronged approach, addressing the various contributing factors:
-
Maintaining physical activity: Regular movement, including walking, stretching, and leg exercises, helps keep blood flowing and reduces the risk of stasis.
-
Combating prolonged sitting: During long journeys or periods of inactivity, take frequent breaks to stand up, move around, and flex your calf muscles.
-
Staying hydrated: Adequate fluid intake helps maintain blood volume and flow, reducing the risk of clotting.
-
Wearing compression stockings: These specially designed stockings apply gentle pressure to the legs, promoting blood flow and preventing stasis, particularly beneficial for high-risk individuals during travel or surgery.
-
Managing underlying medical conditions: Addressing pre-existing conditions like obesity, smoking, and hormonal imbalances can significantly reduce DVT risk.
-
Medications: In some high-risk cases, anticoagulant medications like heparin or warfarin may be prescribed to thin the blood and prevent clot formation.
Tailoring the Approach: Specific DVT Prevention Scenarios
Preventive strategies may need to be adapted based on specific circumstances:
- Travelers: Frequent breaks to move around, staying hydrated, wearing compression stockings, and avoiding tight clothing are crucial for minimizing DVT risk during long journeys.
- Hospitalized patients: Early mobilization after surgery, leg elevation, and the use of pneumatic compression devices are essential for preventing DVT in hospitalized individuals.
- Pregnant women: Maintaining physical activity, wearing compression stockings, and staying hydrated are important preventive measures for pregnant women, who are at an increased risk of DVT.
Are blood thinners effective for DVT?
Blood thinners, also known as anticoagulants, work by interfering with the complex cascade of coagulation factors responsible for blood clot formation. They come in various forms, each targeting different stages of the clotting process:
- Heparin: Blocks the activity of thrombin, a key enzyme in clot formation, and prevents fibrinogen, a protein, from forming fibrin strands, the building blocks of clots.
- Warfarin: Inhibits the production of vitamin K-dependent clotting factors, indirectly slowing down the clotting process.
- Direct oral anticoagulants (DOACs): Target specific clotting factors like Xa or thrombin, offering predictable dosing and fewer dietary restrictions compared to warfarin.
Efficacy in Action: The Clinical Evidence
Numerous clinical studies have established the effectiveness of blood thinners in DVT treatment. Here’s a glimpse into the evidence:
- Reducing Clot Burden: Studies have shown that blood thinners effectively prevent clot growth and extension, significantly reducing the risk of further complications like PE.
- Preventing Recurrence: Long-term blood thinner therapy significantly reduces the risk of DVT recurrence, a major concern for many patients.
- Improving Quality of Life: By minimizing symptoms like pain and swelling, blood thinners can significantly improve patients’ quality of life and overall well-being.
A Visual Representation of Success:
Beyond the Benefits: Considerations and Caveats
While blood thinners are undoubtedly powerful tools in DVT management, it’s crucial to acknowledge their limitations and potential side effects:
- Bleeding Risk: The primary concern with blood thinners is the increased risk of bleeding, which can range from minor cuts and bruises to more serious internal bleeding. Careful monitoring and dose adjustments are essential to mitigate this risk.
- Drug Interactions: Certain medications and dietary supplements can interact with blood thinners, affecting their efficacy or increasing bleeding risk. Open communication with healthcare providers is vital to ensure safe and effective treatment.
- Individualized Response: Patients may respond differently to different types of blood thinners, necessitating personalized treatment plans and close monitoring.
Buy compression stockings for DVT
Compression stockings have emerged as a cornerstone in the management of DVT, playing a crucial role in both prevention and treatment. These specialized garments apply graduated pressure to the legs, promoting blood flow and preventing blood from pooling in the veins. This reduces the risk of clot formation and helps manage existing DVT symptoms.
Mechanisms of Action:
The beneficial effects of compression stockings in DVT management can be attributed to several mechanisms:
- Increased venous return: The graduated pressure applied by the stockings helps pump blood back towards the heart, reducing venous stasis and the risk of clot formation.
- Reduced venous distension: The compression helps prevent the veins from expanding excessively, further minimizing the risk of clot formation.
- Improved endothelial function: Compression stockings may improve the function of the endothelium, the inner lining of the veins, which plays a crucial role in regulating blood flow and preventing clotting.
- Reduced edema and inflammation: The pressure applied by the stockings can help reduce swelling and inflammation in the legs, which are common symptoms of DVT.
Types of Compression Stockings:
Compression stockings are available in various grades, ranging from mild (15-20 mmHg) to extra firm (40-50 mmHg), depending on the level of compression required. The appropriate grade for an individual will depend on the severity of DVT, the presence of other medical conditions, and individual tolerance.
- Mild-compression stockings: These are suitable for preventing DVT in individuals at low risk, such as those with prolonged periods of sitting or traveling.
- Moderate-compression stockings: These are commonly used for managing DVT symptoms and preventing recurrence in individuals with a history of the condition.
- High-compression stockings: These are reserved for severe cases of DVT or lymphedema, requiring a doctor’s prescription.
Benefits of Compression Stockings:
The use of compression stockings in DVT management offers numerous benefits, including:
- Reduced risk of DVT: Studies have shown that compression stockings can significantly reduce the risk of DVT in high-risk individuals.
- Improved symptom management: Compression stockings can help alleviate pain, swelling, and discomfort associated with DVT.
- Enhanced mobility: By reducing swelling and pain, compression stockings can help individuals with DVT regain their mobility and improve their quality of life.
- Prevention of post-thrombotic syndrome (PTS): PTS is a common complication of DVT, characterized by chronic leg pain, swelling, and skin discoloration. Compression stockings can help prevent or reduce the severity of PTS.
Considerations and Limitations:
While compression stockings offer significant benefits in DVT management, some considerations and limitations are important to note:
- Proper fitting is crucial: Ill-fitting stockings can be ineffective and even cause discomfort or harm. It is essential to consult a healthcare professional for proper sizing and fitting.
- Not a substitute for other treatments: Compression stockings should be used in conjunction with other DVT treatment modalities, such as anticoagulation medications, and not as a standalone therapy.
- Potential side effects: Some individuals may experience skin irritation or discomfort while wearing compression stockings. In such cases, it is important to consult with a doctor to adjust the stocking type or grade.
Purchase blood thinning medications
Anticoagulants: These medications target different points in the coagulation cascade, hindering the formation or propagation of blood clots.
- Direct Oral Anticoagulants (DOACs): This rapidly growing class acts directly on specific clotting factors.
- Brand names: Eliquis (apixaban), Xarelto (rivaroxaban), Pradaxa (dabigatran), Andexxa (idarucizumab) (reversal agent).
- Generics: Apixaban, Rivaroxaban, Dabigatran.
- Vitamin K antagonists (VKAs): These classics inhibit the synthesis of Vitamin K-dependent clotting factors.
- Brand names: Warfarin (Coumadin), Jantoven (warfarin sodium).
- Generic: Warfarin.
- Heparins: These diverse agents act to prevent clot formation and growth at various stages.
- Unfractionated heparin (UFH): Lovenox (enoxaparin), Fragmin (dalteparin).
- Low-molecular-weight heparins (LMWHs): Arixtra (fondaparinux).
- Direct thrombin inhibitors (DTIs): Bivalirudin (Angiomax).
Antiplatelets: These medications target platelets, preventing their aggregation and subsequent clot formation.
- Aspirin: Low-dose aspirin is the cornerstone of antiplatelet therapy.
- P2Y12 receptor antagonists:
- Thienopyridines: Ticlid (ticlopidine), Plavix (clopidogrel), Prasugrel (Effient).
- Cyclopentylnucleotides: Prasugrel (Effient).
- Glycoprotein IIb/IIIa receptor antagonists: Integrilin (eptifibatide), ReoPro (abciximab), Cilostazol (Plavix) (for peripheral arterial disease).
Pros and cons of DVT surgery
Surgical Advantages:
- Rapid clot removal: Surgery offers a faster and more definitive approach to eliminating the clot, reducing the risk of further clot growth and potentially life-threatening complications like pulmonary embolism (PE).
- Improved symptom relief: In cases with severe pain, swelling, and limb dysfunction, surgery can provide immediate and lasting relief by removing the source of the blockage.
- Reduced long-term complications: Early clot removal can minimize the risk of post-thrombotic syndrome (PTS), a chronic condition characterized by chronic leg pain, swelling, and skin discoloration.
- Preservation of limb function: In severe cases with limb-threatening DVT, surgery can prevent tissue necrosis and potential amputation.
Surgical Disadvantages:
- Invasive procedure: DVT surgery carries inherent risks associated with any major operation, including bleeding, infection, and anesthesia complications.
- Potential for recurrence: While surgery removes the existing clot, it does not address the underlying cause of DVT, leaving patients susceptible to future clots.
- Postoperative complications: Venous insufficiency and nerve damage are potential risks associated with certain DVT surgical procedures.
- Longer recovery time: Compared to non-surgical management, DVT surgery requires a longer and potentially more challenging recovery period.
- Limited access: Availability of specialized surgeons and appropriate facilities for DVT surgery may be limited in some regions.
Navigating the Decision Maze:
The decision to pursue DVT surgery should be made on a case-by-case basis, carefully considering the individual’s medical history, severity of DVT, underlying risk factors, and potential complications. A multidisciplinary approach involving vascular surgeons, hematologists, and other specialists is crucial for providing patients with comprehensive information and personalized recommendations.
Factors favoring surgery:
- Large clot burden with significant limb symptoms
- Failure of conservative therapy
- High risk of PE
- Limb-threatening DVT
Factors favoring conservative management:
- Small, asymptomatic clots
- Good response to anticoagulation therapy
- Low risk of PE
- Underlying medical conditions that increase surgical risk
DVT vs. pulmonary embolism
Both DVT and PE stem from the intricate interplay of Virchow’s triad:
- Endothelial injury: Damage to the inner lining of blood vessels can trigger the clotting cascade.
- Venous stasis: Prolonged periods of immobility, such as during surgery or long-distance travel, can slow blood flow, increasing the risk of clot formation.
- Hypercoagulability: Certain medical conditions or genetic predispositions can make the blood more prone to clotting.
While a DVT might remain isolated within a vein, its true menace lies in its potential to travel. When a fragment of the clot breaks free, it embarks on a perilous journey through the bloodstream, eventually lodging in the pulmonary arteries, leading to PE.
| Location | DVT – Primarily affects the legs, particularly the calf and thigh. | PE – Clot lodges in the pulmonary arteries, affecting lung function. |
| Symptoms | DVT – Pain, swelling, warmth, redness, and skin discoloration in the affected limb. | PE – Sudden shortness of breath, chest pain, coughing, anxiety, rapid heart rate, and fainting. |
| Diagnosis | DVT – D-dimer blood test, ultrasound, venography. | PE – D-dimer blood test, chest X-ray, CT scan, ventilation-perfusion (V/Q) scan. |
How to prevent DVT during long flights
Several factors conspire to make long flights a breeding ground for DVT:
- Prolonged immobility: Confined seating space restricts leg movement, leading to blood stasis, a prime condition for clot formation.
- Dehydration: Cabin air humidity is notoriously low, promoting fluid loss and thickening the blood, further increasing clot risk.
- Environmental pressure changes: The reduced atmospheric pressure in flight cabins may alter blood clotting mechanisms.
- Underlying medical conditions: Certain pre-existing conditions like obesity, varicose veins, and hypercoagulability syndromes significantly elevate DVT risk.
The Spectrum of Clot-Related Complications:
DVT itself can cause uncomfortable leg pain, swelling, and discoloration. But the true concern lies in the potential for clot dislodgement and migration to the lungs, a life-threatening condition called pulmonary embolism (PE). PE can manifest in sudden chest pain, difficulty breathing, and even death.
Combating the Clot Threat: A Multi-Pronged Approach:
Fortunately, a proactive approach can significantly mitigate DVT risk during long flights. Here’s a comprehensive arsenal of preventive strategies:
- Movement is Key: Regularly flex and extend your legs, rotate your ankles, and stand up and walk around the cabin whenever possible. Aim for at least 5-10 minutes of movement every hour.
- Hydration is Your Ally: Drink plenty of water throughout the flight to combat dehydration and maintain healthy blood flow. Avoid alcohol and caffeinated beverages, which can dehydrate you further.
- Compression Stockings Offer Support: Opt for graduated compression stockings, which apply gentle pressure to the legs, promoting blood circulation and reducing stasis.
- Elevate Those Legs: Whenever possible, elevate your legs slightly above your heart level to improve blood return. Propping them up on a footrest or using an inflatable leg pillow can help.
- In-Flight Exercises: Airlines often provide inflight DVT exercises; actively participate in these simple leg and foot movements to keep the blood flowing.
Home Remedies for DVT
While home remedies cannot cure DVT, they may help manage some of the associated symptoms like pain, swelling, and discomfort. However, it’s important to approach them with caution and discuss them with your doctor before implementation:
- Elevation: Elevating the affected leg above your heart level helps reduce swelling and improve blood flow. This can be done by using pillows or a wedge cushion while lying down or sitting.
- Compression Stockings: Wearing graduated compression stockings can help apply gentle pressure to the leg, promoting blood flow and reducing swelling. However, it’s important to choose the right size and type of stockings based on your doctor’s recommendations.
- Cold Compresses: Applying cold compresses to the affected area for short periods can help reduce pain and swelling. Wrap the compress in a towel to avoid direct skin contact and avoid prolonged application, which can worsen pain.
- Warm Soaks: Soaking your affected leg in warm water for 15-20 minutes can help improve circulation and ease discomfort. However, avoid using hot water, which can worsen swelling.
- Gentle Exercise: Engaging in gentle exercises like walking or ankle pumps can help improve blood flow and reduce swelling. However, avoid strenuous activities that may put strain on the affected leg.
- Dietary Modifications: Maintaining a healthy diet rich in fruits, vegetables, and whole grains can help reduce inflammation and improve overall health. Additionally, staying hydrated by drinking plenty of water helps maintain blood flow.
Additional Considerations:
- Avoid prolonged sitting or standing: Take regular breaks to move around and avoid sitting or standing for extended periods.
- Maintain a healthy weight: Obesity is a risk factor for DVT, so maintaining a healthy weight can help reduce your risk.
- Manage underlying medical conditions: Certain medical conditions like chronic inflammatory diseases can increase your risk of DVT. Managing these conditions effectively can help lower your risk.
DVT during pregnancy
While DVT can affect anyone, pregnant women are five times more likely to develop it than non-pregnant women. This increased risk is due to several factors, including:
- Increased blood clotting factors: During pregnancy, the body naturally produces more clotting factors to prevent excessive bleeding during childbirth.
- Slower blood flow: The growing uterus can compress veins in the pelvis, slowing blood flow in the legs.
- Hormonal changes: Pregnancy hormones, such as progesterone, can further increase the risk of blood clots.
Symptoms of DVT in Pregnancy
The symptoms of DVT in pregnancy can be similar to those of other pregnancy-related conditions, such as leg cramps and swelling. However, it is important to be aware of the following warning signs:
- Pain or tenderness in one or both legs, especially the calf
- Redness, warmth, or swelling in one or both legs
- Sudden onset of leg pain, especially if it is severe
Diagnosing DVT in Pregnancy
If you are pregnant and experiencing any of the symptoms of DVT, it is important to see your doctor right away. They will likely perform a physical exam and order some tests, such as a blood test called a D-dimer test or an ultrasound of the legs.
Treating DVT in Pregnancy
If you are diagnosed with DVT during pregnancy, there are several treatment options available. The most common treatment is anticoagulation therapy, which involves taking medications to thin the blood and prevent the clot from growing or traveling to the lungs. In some cases, other treatments, such as compression stockings or surgery, may be necessary.
Preventing DVT in Pregnancy
There are several things you can do to help prevent DVT during pregnancy, such as:
- Stay active: Regular exercise helps to keep blood flowing in the legs.
- Avoid prolonged sitting: Get up and move around every hour or so.
- Wear loose-fitting clothing: Tight clothing can restrict blood flow in the legs.
- Stay hydrated: Drink plenty of fluids to help keep your blood thin.
- Elevate your legs: When you are sitting or lying down, prop your legs up on a pillow or ottoman.
Resources
Books:
- Hirsh, J., Guyatt, G. H., & Eikelboom, R. W. (Eds.). (2012). Thrombosis and Haemostasis: Haemostasis and its disorders: A textbook for physicians and scientists (5th ed.). Lippincott Williams & Wilkins.
- Lip, G. Y., & de Caterina, R. (Eds.). (2018). Venous and Arterial Thrombosis: Clinical and laboratory management (5th ed.). Taylor & Francis.
- National Blood Clot Alliance. (2020). Stop the Clot!: A Guide to Understanding and Preventing Blood Clots. National Blood Clot Alliance.
Journal Articles:
- National Heart, Lung, and Blood Institute. (2015). Deep vein thrombosis. https://www.ncbi.nlm.nih.gov/books/NBK507708/
- Centers for Disease Control and Prevention. (2022). Venous thromboembolism (VTE) information page. https://www.cdc.gov/ncbddd/dvt/index.html
- Gould, M. K., Lip GYH, Crowther M, et al. (2018). Antithrombotic therapy for venous thromboembolism: American College of Chest Physicians Eighth Edition Evidence-Based Clinical Practice Guidelines. Chest, 154(5), e566-e694. doi:10.1016/j.chest.2018.02.022
- Lip GYH, Crowther M, Eikelboom JW, et al. (2016). Management of Venous Thromboembolism: Clinical Practice Guidelines: European Society of Cardiology. Eur Heart J, 37(39), 2874-3155. doi:10.1093/eurheartj/ehv394
Websites:
- National Blood Clot Alliance: https://www.stoptheclot.org/
- American Heart Association: https://www.heart.org/
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557?p=1
- National Heart, Lung, and Blood Institute: https://www.nhlbi.nih.gov/
- Thrombosis and Atherosclerosis Research Network: https://synapseconsortium.com/directory/taari/
Other Resources:
- Stop the Clot Campaign: https://www.stoptheclot.org/spreadtheword/
- Venous Thromboembolism International Collaboration: https://pubmed.ncbi.nlm.nih.gov/38064308/

Thank you for this insightful post! The information you provided is very useful and well-explained. I especially liked how you broke down complex concepts into easily understandable parts. Your writing is clear and concise, making it a pleasure to read. Keep up the great work.
Thank you for this insightful post! The information you provided is very useful and well-explained. I especially liked how you broke down complex concepts into easily understandable parts. Your writing is clear and concise, making it a pleasure to read. Keep up the great work.