TOC
- 1 What is herpes?
- 2 Understanding Herpes: An Overview
- 3 Best herpes treatment
- 4 Herpes test kits
- 5 What is difference between Herpes vs. HPV
- 6 What is Acyclovir vs. valacyclovir Treatment for herpes
- 7 What are Oral vs. genital herpes
- 8 Herpes support groups
- 9 Home remedies for herpes
- 10 Herpes vaccines
- 11 Resources
What is herpes?
Herpes, a group of viruses causing painful blisters and ulcers, has plagued humanity for millennia. Tracing its history reveals a fascinating journey of medical understanding, evolving from ancient observations to modern scientific advancements.
Early Glimmers:
- Ancient Egypt (1550 BC): The Ebers Papyrus, one of the oldest medical texts, mentions skin lesions resembling herpes, suggesting awareness of the condition in ancient times.
- Ancient Greece (5th century BC): Hippocrates, the “father of medicine,” described blisters on the genitals, potentially referring to genital herpes.
- Roman Empire (1st century AD): Emperor Tiberius reportedly banned kissing due to widespread cold sores, hinting at the prevalence of oral herpes.
Medieval Obscuration:
- During the Middle Ages, with limited medical knowledge and emphasis on religious explanations, detailed documentation of herpes appears scarce.
Renaissance Recognition:
- 16th century: The term “herpes” originates from the Greek word “herpein,” meaning “to creep,” reflecting the characteristic spreading of blisters.
- 18th century: Italian physician Giovanni Coeli describes genital herpes in detail, paving the way for more accurate diagnosis and understanding.
Modern Discoveries:
- 1919: American scientist Peter Paul Airola experimentally proves the infectious nature of herpes, dispelling earlier theories of spontaneous eruptions.
- 1925: Japanese ophthalmologist Hideyo Noguchi successfully isolates the herpes simplex virus (HSV) under a microscope, marking a significant breakthrough.
- 1940s: Development of the first antiviral medication, acyclovir, revolutionizes herpes treatment, offering relief and reducing outbreak severity.
- 21st century: Ongoing research delves deeper into the complex biology of herpesviruses, exploring potential vaccines and gene therapy approaches for long-term management.
The Long Shadow of Herpes:
Despite advancements, herpes remains a global health concern.
- Millions worldwide live with HSV-1 and HSV-2, the most common herpesviruses.
- Stigma and misinformation surrounding herpes persist, creating emotional and social challenges for individuals affected.
Understanding Herpes: An Overview
Herpes is a common viral infection caused by two types of viruses: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). HSV-1 is primarily responsible for oral herpes, which can cause sores on the mouth and around the lips, commonly known as cold sores. HSV-2, on the other hand, typically causes genital herpes, a sexually transmitted infection characterized by sores or blisters in the genital area.
Despite the different locations, both forms of herpes can cause sores in either the oral or genital areas, as well as in other parts of the body. The virus is highly contagious and can be transmitted from one person to another through direct contact with a herpes sore, saliva (even if the person is asymptomatic), or skin contact in the genital area.
While most people with herpes do not exhibit any symptoms, those who do may experience painful blisters or ulcers at the infection site, fever, body aches, and swollen lymph nodes during the first outbreak. Recurrent outbreaks are usually less severe and occur less frequently over time.
There is currently no cure for herpes, but there are antiviral medications that can help manage symptoms, reduce the severity of outbreaks, and lower the risk of transmitting the virus to others.
Understanding herpes and its transmission is crucial for prevention. Having regular check-ups, practicing safe sex, and avoiding direct contact with sores can significantly reduce the risk of getting or spreading herpes.
Herpes symptoms
- Tingling or itching: Before blisters appear, you may feel tingling, itching, or burning sensations in the affected area.
- Blisters: The hallmark symptom of herpes is the formation of small, fluid-filled blisters that cluster together. These blisters can be painful and break open, forming scabs.
- Fever, fatigue, and swollen lymph nodes: During the initial infection, you may experience fever, fatigue, and swollen lymph nodes.
- Painful urination: Genital herpes can also cause pain during urination.
- Genital discharge: In some cases, genital herpes can cause vaginal or urethral discharge.
Types of herpes
- HSV-1: This strain primarily causes oral herpes, also known as cold sores. It can also infect the genitals through oral-genital contact.
- HSV-2: This strain primarily causes genital herpes, but it can also infect the mouth through oral-genital contact.
- Stages of herpes infection
Primary infection: This is the first time you contract the virus. Symptoms usually appear within 2-12 days after exposure and can last for several weeks.
- Latency: After the initial outbreak, the virus becomes dormant in nerve cells. You may not experience any symptoms during this stage.
- Recurrence: The virus can reactivate and cause outbreaks, often triggered by stress, illness, or other factors. Recurrences are usually milder than the initial infection.
- Herpes causes
- Skin-to-skin contact: Herpes is transmitted through direct skin-to-skin contact with an infected person, even if they don’t have visible blisters.
- Sharing personal items: Sharing razors, towels, or other personal items contaminated with the virus can also spread herpes.
- Oral-genital contact: Oral-genital contact can transmit HSV-1 and HSV-2 between partners.
Best herpes treatment
Unfortunately, there’s no “one-size-fits-all” cure for herpes. The best treatment approach depends on several factors, including the type of herpes (HSV-1 or HSV-2), the severity of your symptoms, and your individual medical history. However, some general principles apply:
- Antiviral medications: These drugs like acyclovir, valacyclovir, and famciclovir can shorten the duration and severity of outbreaks, reduce the risk of transmission, and prevent recurrences. They can be taken episodically (when you feel an outbreak coming on) or suppressively (daily to prevent outbreaks).
- Pain relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage discomfort during outbreaks.
- Topical creams: Over-the-counter creams like docosanol (Abreva) can shorten the healing time of cold sores.
Top herpes creams
While prescription and over-the-counter medications are crucial, topical creams can offer additional relief:
- Abreva: This docosanol cream is proven to shorten the healing time of cold sores.
- Zostrix: This cream, containing capsaicin, acts as a local anesthetic to numb pain.
- Calamine lotion: This soothing lotion can provide temporary relief from itching and burning.
Herpes management products
Beyond medication, several products can help you manage your condition:
- Cold sore patches: These adhesive patches act as a barrier to prevent picking and reduce the risk of spreading the virus.
- Ice packs: Applying ice packs to cold sores can provide temporary pain relief.
- Stress management techniques: Stress can trigger outbreaks, so practices like meditation or yoga can help manage stress and potentially reduce recurrences.
Herpes test kits
- Blood test: These kits, available online or in pharmacies, typically require you to prick your finger and collect a few drops of blood. They detect antibodies to the herpes virus, indicating past exposure, but cannot differentiate between HSV-1 (oral herpes) and HSV-2 (genital herpes).
- Swab test: These kits involve collecting a swab from the suspected blister or lesion. The swab is then mailed to a lab for analysis to detect the presence of the herpes virus DNA. This method can distinguish between HSV-1 and HSV-2.
- Combination test: Some kits offer both a blood test and a swab test, providing a more comprehensive picture of your exposure.
Key Considerations when Choosing a Herpes Test Kit:
- Accuracy: Look for kits from reputable brands with high accuracy rates.
- Type of herpes detected: Decide if you need to differentiate between HSV-1 and HSV-2.
- Convenience: Consider kit format (finger prick vs. swab) and turnaround time for results.
- Cost: Prices vary depending on type, features, and retailer.
- Privacy: Check the kit’s privacy policy to ensure your results are confidential.
Popular Herpes Test Kit Options:
- EverlyWell: Offers both blood and swab tests with fast turnaround times and online consultations with healthcare professionals.
- LetsGetChecked: Provides various test options, including combination kits, and prioritizes discreet packaging and online support.
- iCare Herpes-2 Test Kit: This FDA-approved kit offers a self-contained swab test for detecting HSV-2 only.
- myLAB Box My Lab Box 5 Panel STD Test: This comprehensive kit tests for multiple STIs, including herpes, and provides discreet shipping and online doctor consultations.
What is difference between Herpes vs. HPV
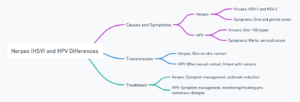
Herpes (HSV) and HPV are two distinct viruses:
- Causes and Symptoms:
- Herpes is primarily caused by two types of viruses: HSV-1 and HSV-2, leading to oral and genital sores.
- HPV encompasses over 100 viruses, causing conditions from warts on various body parts to more serious outcomes like cervical cancer.
- Transmission: Both can be transmitted through skin-to-skin contact, but HPV is often more associated with sexual contact and has a strong link with cervical and other cancers.
- Treatment: There’s no cure for either virus, but treatments for herpes focus on managing symptoms and reducing outbreaks, while HPV treatment revolves around managing symptoms and, in the case of high-risk types, monitoring and treating pre-cancerous changes.
What is Acyclovir vs. valacyclovir Treatment for herpes
-
Acyclovir and valacyclovir are both antiviral medications used to treat herpes infections. While they share some similarities, there are also key differences between them:
Effectiveness:
- Both medications are effective in treating herpes outbreaks, including genital herpes, cold sores, and shingles.
- Studies have shown no significant difference in their effectiveness for treating first-episode genital herpes.
- Valacyclovir may be slightly more effective for relieving pain and shortening the duration of shingles compared to acyclovir.
Dosage:
- Acyclovir requires more frequent dosing, typically five times a day, due to its lower bioavailability.
- Valacyclovir is much better absorbed by the body, allowing for less frequent dosing, typically two or three times a day.
Convenience:
- Valacyclovir’s simpler dosing schedule may lead to better adherence, which can ultimately improve treatment outcomes.
- For some people, the reduced pill burden of valacyclovir may be a significant advantage.
Cost:
- Valacyclovir is typically more expensive than acyclovir.
Side effects:
- Both medications are generally well-tolerated, with side effects like headache, nausea, and fatigue being most common.
- These side effects are usually mild and transient.
Overall:
- Both acyclovir and valacyclovir are effective options for treating herpes.
- Valacyclovir’s advantages include a simpler dosing schedule, potentially better adherence, and possible benefits for treating shingles.
- However, acyclovir may be a more cost-effective option for some people.
What are Oral vs. genital herpes
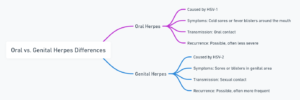
Virus:
- Oral herpes: Usually caused by HSV-1 (herpes simplex virus type 1), but can also be caused by HSV-2 (less common).
- Genital herpes: Primarily caused by HSV-2, but can also be transmitted by HSV-1 (through oral-genital contact).
Symptoms:
- Oral herpes: Presents as cold sores or fever blisters typically around the mouth and lips, but can also occur on the inside of the mouth, chin, and cheeks. Symptoms include tingling, itching, burning, and painful blisters that eventually crust over.
- Genital herpes: Presents as blisters or ulcers on the genitals, buttocks, and surrounding areas. Blisters can also appear on the thighs, groin, and anus. Similar to oral herpes, symptoms include tingling, itching, burning, and pain.
Transmission:
- Oral herpes: Primarily transmitted through close contact, such as kissing or sharing utensils, when someone has an active sore or even during asymptomatic shedding of the virus.
- Genital herpes: Transmitted through skin-to-skin contact with infected areas during vaginal, anal, or oral sex. Sharing sex toys can also be a risk.
Frequency and severity of outbreaks:
- Oral herpes: Outbreaks tend to be more frequent in the first year of infection but gradually become less frequent over time. They are usually less severe than genital herpes outbreaks.
- Genital herpes: Outbreaks can be more frequent and severe, especially in the first year after infection. They can also be more painful and have a longer healing time.
Long-term implications:
- Both oral and genital herpes are lifelong infections, but the virus lays dormant in most people between outbreaks.
- Genital herpes can have additional risks, such as increased risk of complications during pregnancy and childbirth.
Here are some additional points to remember:
- There is no cure for herpes, but medication can help manage outbreaks and reduce their severity.
- It is possible to have both oral and genital herpes.
-
- Safe sex practices, such as using condoms, can help reduce the risk of transmitting genital herpes.
Herpes support groups
- ASHA’s STI Support Forum: Hosted on Inspire.com, this forum allows you to connect with others anonymously and discuss various aspects of living with herpes, from managing outbreaks to navigating relationships.
- Positive Singles: This online community specifically caters to singles living with herpes and offers forums, chat rooms, and events to help you build connections and find love.
- Herpes Support Network: This website provides a directory of online and in-person herpes support groups around the world, making it easier to find a group near you.
Home remedies for herpes

Here are the details of each remedy:
- Cold Compress: Applying a cold compress or ice pack can help reduce swelling and pain associated with herpes sores.
- Warm Baths: Taking warm baths can soothe the sores and help keep the affected area clean and dry.
- Pain Relievers: Over-the-counter pain relievers can help reduce discomfort during outbreaks.
- Loose Clothing: Wearing loose-fitting clothing can prevent irritation of the sores and promote healing.
- Dietary Changes: Boosting the immune system by eating a healthy diet and avoiding arginine-rich foods can help manage outbreaks.
- Herbal Treatments: Applying herbal treatments like aloe vera or tea tree oil topically can provide relief and aid in healing.
Preventing herpes transmission
- Practice Safe Sex: Use condoms and dental dams during sexual activity to reduce the risk of transmission. Note that while these reduce the risk, they do not eliminate it entirely due to potential skin contact.
- Avoid Sexual Activity During Outbreaks: Refrain from sexual contact (including oral, vaginal, and anal sex) when symptoms or outbreaks of herpes are present.
- Communicate with Partners: Have open and honest discussions about STDs with sexual partners. Sharing herpes status allows partners to make informed decisions and take precautions.
- Use Antiviral Medications: For those diagnosed with herpes, daily antiviral medication can reduce the likelihood of transmission to partners.
- Know the Signs: Be aware of the early symptoms of herpes outbreaks, such as tingling, itching, or pain in affected areas, and take precautions during these times.
- Limit the Number of Sexual Partners: Reducing the number of sexual partners decreases the overall risk of STD transmission, including herpes.
- Get Regular STD Check-ups: Regular screenings for STDs help ensure early detection and management of herpes and other conditions.
- Avoid Sharing Personal Items: Do not share items that come into contact with sores, such as lip balm, towels, or utensils, especially during an outbreak.
- Maintain General Health and Immunity: A healthy immune system can help manage and reduce the frequency of outbreaks, potentially reducing the risk of transmission.
- Educate Yourself and Others: Understanding herpes and its transmission can empower you and others to take appropriate preventive measures.
Herpes vaccines
As of the latest available information, there are no authorized or commercially available vaccines for the prevention of herpes simplex virus (HSV) infections. Research and clinical trials are ongoing for several potential vaccine candidates, but none have completed the necessary phases of development and approval to become available to the public. However, multiple herpes vaccine candidates are in clinical research, using various technologies like DNA, mRNA, and protein subunits.
- BioNTech’s BNT163: An mRNA vaccine targeting HSV-2 and potentially HSV-1, aimed at preventing cellular entry and immunosuppression.
- Moderna’s mRNA-1608: Aims to induce a strong immune response, combining antibody and cell-mediated immunity.
- Completion Dates: Many of these trials, including those for BNT163 and mRNA-1608, are expected to complete around June 2025.
- No Current Authorization: As of the latest updates, no herpes vaccines have been authorized by major health agencies.
Resources
- Gene Therapy Trial for Herpes: https://www.sciencedaily.com/releases/2020/08/200818094019.htm
- New Antiviral Molecule for Herpes: https://studyfinds.org/new-drug-covid-19-and-herpes/
- Promising Herpes Vaccine Research: https://www.nature.com/subjects/herpes-virus/nature
- Microdosing Antivirals for Herpes: https://www.sciencedirect.com/science/article/pii/S187962571600016X

