Pain Measurement Scales are crucial tools in both clinical and research settings, providing a standardized method for assessing pain, an inherently subjective experience. These scales, ranging from the simple Numerical Rating Scale (NRS) to the more comprehensive McGill Pain Questionnaire (MPQ), serve as vital communication bridges between patients and healthcare providers. They not only aid in accurately gauging the intensity of pain but also in understanding its nature and impact on an individual’s daily life. Our exploration into these scales will delve into how they are used, their significance, and the differences among them, offering a clearer understanding of this essential aspect of pain management. Here are some of the different scales used to measure pain:
TOC
Numerical Rating Scales (NRS):

-
NRS (Numerical Rating Scales) are simple, yet effective tools for measuring pain intensity. They consist of a numbered line (usually 0-10) with descriptive anchors at either end (e.g., “no pain” and “worst pain imaginable”). Patients simply choose the number that best represents their current pain level.
When to Use NRS:
- Acute Pain: NRS are ideal for assessing pain in acute settings like emergency departments, post-surgery, or trauma centers. Their simplicity makes them quick and easy to administer.
- Chronic Pain: NRS can also be used to monitor chronic pain, especially when tracking changes in intensity over time.
- Diverse Populations: NRS are language and culture-independent, making them suitable for use with patients who may have difficulty communicating verbally.
Ideal Patient for NRS:
- Capable of understanding numbers and basic descriptors of pain intensity.
- Able to communicate their pain level clearly.
- Free from cognitive impairment or other factors that may interfere with accurate reporting.
Pros:
- Easy to administer and understand.
- Quick and efficient to use.
- Reliable and valid for measuring pain intensity.
- Sensitive to changes in pain level.
- Language and culture-independent.
- Widely accepted and used in healthcare settings.
Cons:
- Limited ability to capture the multidimensional nature of pain (e.g., quality, location).
- May not be suitable for all patients, particularly those with cognitive impairment or communication difficulties.
- Subjective and prone to individual variations in interpretation of numbers and pain descriptors.
- Potential for recall bias, especially when assessing chronic pain.
Overall, NRS are valuable tools for pain assessment in many clinical settings. However, it’s important to consider their limitations and use them in conjunction with other pain assessment methods for a more comprehensive understanding of a patient’s pain experience.
Visual Analog Scale (VAS):

- A horizontal line ranging from 0 to 10, with 0 being no pain and 10 being the worst pain imaginable. Patients mark a point on the line to indicate the severity of their pain.
Ideal situations:
- Measuring subjective experiences: VAS is best suited for subjective experiences like pain, anxiety, fatigue, or nausea, where objective assessment is difficult.
- Continuous data: VAS provides continuous data, allowing for finer-grained analysis of changes in intensity compared to discrete scales.
- Simple and quick: Easy to understand and use for both patients and healthcare providers.
- Minimal language dependence: Can be used with patients who have limited language skills or communication difficulties.
Specific applications:
- Pain management: Monitoring pain severity over time and evaluating treatment effectiveness.
- Palliative care: Assessing symptom burden and response to interventions.
- Mental health: Measuring anxiety, depression, and other symptoms.
- Research: Capturing subjective experiences in clinical trials and epidemiological studies.
Ideal patient for VAS:
- Cooperative and able to understand instructions: Can accurately mark the line based on their experience.
- Able to communicate their pain or discomfort: Can explain the location and intensity of their symptoms if needed.
- Has a stable hand and good visual acuity: Can accurately mark the line without difficulty.
Pros of VAS:
- Sensitivity: Detects small changes in symptom intensity.
- Responsiveness: Captures changes over time and treatment effects.
- Versatility: Can be used for various subjective experiences.
- Simplicity and ease of use: Requires minimal training and explanation.
- Minimal language dependence: Can be used with diverse populations.
Cons of VAS:
- Subjectivity: Relies on individual interpretation and can be influenced by personal factors.
- Accuracy: Requires good comprehension and communication skills to mark the line accurately.
- Cultural bias: Anchor terms might not translate well across cultures.
- Floor and ceiling effects: Patients might cluster at the ends of the scale, limiting the data’s range.
- Training required: Healthcare providers need to understand how to interpret VAS scores.
Overall, VAS is a valuable tool for measuring subjective experiences in various clinical and research settings. However, it’s important to consider the limitations and choose the most appropriate scale based on the patient and the specific context.
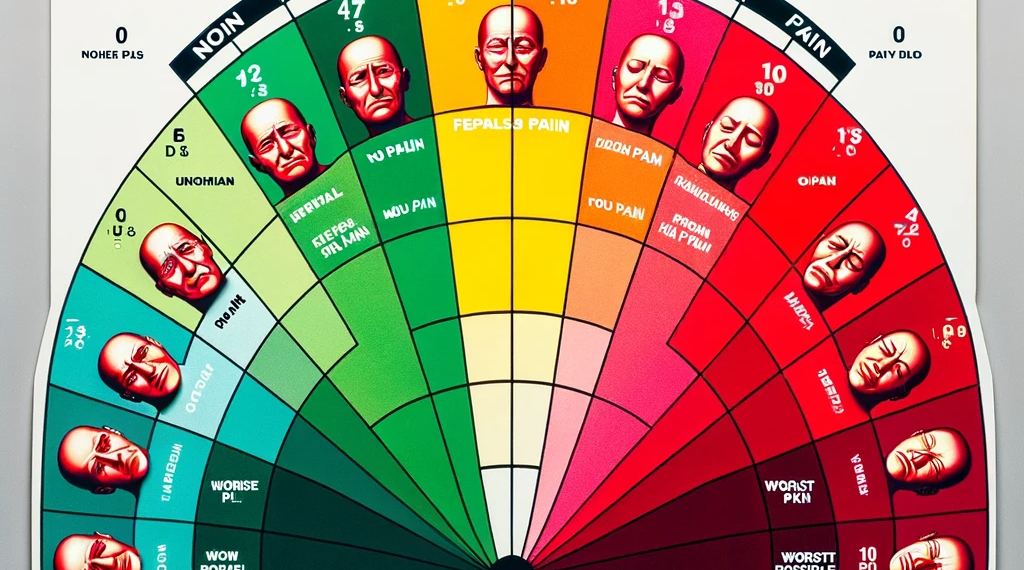
Faces Pain Scale – Revised (FPS-R):

- A series of faces with different expressions, ranging from happy (no pain) to crying (severe pain). Patients choose the face that best represents their pain.
When to use the Faces Pain Scale – Revised (FPS-R):
- The FPS-R is a pain assessment tool that can be used in a variety of settings, including hospitals, clinics, and home care.
- It is particularly useful for assessing pain in children, adults with cognitive or communication impairments, and people who are unable to speak English.
Ideal patient for the Faces Pain Scale – Revised (FPS-R):
- The FPS-R is ideal for patients who:
- Are 3 years of age or older
- Can understand and respond to simple instructions
- Are able to point to or circle a picture that represents their level of pain
Pros of the Faces Pain Scale – Revised (FPS-R):
- The FPS-R is a simple and easy-to-use tool that can be quickly administered.
- It is reliable and valid for measuring pain in a variety of populations.
- The FPS-R is culturally neutral and can be used with people from different backgrounds.
- It is free to use and can be downloaded from the website of the American Pain Society.
Cons of the Faces Pain Scale – Revised (FPS-R):
- The FPS-R may not be accurate for all patients, such as those with severe cognitive or communication impairments.
- Some patients may find the faces to be scary or upsetting.
- The FPS-R is not as sensitive as some other pain assessment tools, such as the Numeric Rating Scale (NRS).
Overall, the Faces Pain Scale – Revised (FPS-R) is a valuable tool for assessing pain in a variety of settings. It is simple to use, reliable, valid, and culturally neutral. However, it is important to be aware of the limitations of the FPS-R and to use it in conjunction with other pain assessment tools when necessary.
Wong-Baker FACES Pain Rating Scale:

- Similar to the FPS-R, but with six faces instead of five. The Wong-Baker FACES Pain Rating Scale is a simple and effective tool used to assess pain intensity in individuals who may have difficulty communicating their pain verbally. It features a series of six faces, ranging from a smiling face representing “No Hurt” to a crying face representing “Hurts the Worst.”
When to Use:
- Children: FACES is particularly helpful for children aged 3 and above who may not understand or be able to use a numerical pain scale.
- Non-verbal individuals: This scale is beneficial for individuals with cognitive or communication impairments, such as those with dementia, autism, or intellectual disabilities.
- Language barriers: FACES can overcome language barriers and facilitate pain assessment in patients who do not speak the same language as the healthcare provider.
- Acute or chronic pain: FACES can be used to assess both acute and chronic pain across various settings, including hospitals, clinics, and home care.
Ideal Patient:
- Individuals who have difficulty communicating their pain verbally.
- Children aged 3 and above.
- Individuals with cognitive or communication impairments.
- Patients with language barriers.
- Individuals experiencing acute or chronic pain.
Pros:
- Simple and easy to understand: The use of facial expressions makes it intuitive for individuals of all ages and cognitive abilities.
- Non-verbal: FACES eliminates the need for verbal communication, making it ideal for non-verbal individuals.
- Culturally neutral: The use of facial expressions transcends cultural differences, making it suitable for diverse populations.
- Widely accepted and used: FACES is a well-established and widely accepted pain assessment tool in various healthcare settings.
- Relatively inexpensive: FACES can be easily reproduced and implemented without significant cost.
Cons:
- Subjectivity: Pain perception is subjective, and individual interpretations of the faces may vary.
- Limited sensitivity: FACES may not be sensitive enough to detect subtle changes in pain intensity, particularly in individuals with chronic pain.
- Developmental limitations: Younger children may not fully understand the concept of pain intensity and may point to random faces.
- Cultural influences: Facial expressions can have different meanings in different cultures, potentially affecting interpretation.
- Limited information: FACES only provides information about pain intensity and lacks details about the pain location or quality.
Overall, the Wong-Baker FACES Pain Rating Scale is a valuable tool for assessing pain in individuals who may have difficulty communicating verbally. Its simplicity, non-verbal nature, and cultural neutrality make it a versatile and accessible option for various healthcare settings. However, it is important to be aware of its limitations and consider using it in conjunction with other pain assessment tools for a more comprehensive evaluation.
FLACC Pain Scale:

- Designed for children who are unable to communicate their pain verbally. The scale assesses five behavioral indicators: facial expression, leg position, activity level, crying, and consolability.
When to Use:
- Pre-verbal children and infants: This scale relies on objective observations rather than self-reporting, making it ideal for non-communicative patients.
- Critically ill or sedated patients: Similarly, patients who cannot easily express pain verbally can be assessed using FLACC.
- Patients with cognitive impairments: Dementia, developmental delays, or other cognitive issues can affect pain communication, making FLACC a valuable tool.
- Acute or chronic pain: The scale can be used for both short-term and long-term pain management, helping track changes and adjust treatment accordingly.
Ideal Patient:
- Non-verbal or unable to communicate effectively: This is the core population for which the FLACC scale was designed.
- Patients with limited mobility or awareness: Observing facial grimacing, changes in muscle tone, and consolability can be helpful in these cases.
- Patients undergoing painful procedures: Monitoring pain during and after procedures can guide interventions and improve patient comfort.
Pros:
- Objective and observer-based: Reduces reliance on self-reporting, leading to potentially more accurate pain assessment.
- Simple and quick to use: Requires minimal training and can be administered in under a minute.
- Widely used and accepted: Familiar to healthcare professionals across various settings.
- Sensitive to changes in pain: Can detect subtle variations in pain levels over time.
Cons:
- Subjective interpretation: Observer bias can influence scoring, requiring careful training and consistent application.
- Limited information: Doesn’t capture the quality or nature of pain like some self-reporting scales.
- Not suitable for all patients: May not be accurate for verbal patients or those with specific conditions.
- Requires ongoing monitoring: Frequent assessments are necessary for effective pain management.
Overall, the FLACC pain scale is a valuable tool for assessing pain in non-verbal or communication-impaired patients. However, it’s important to be aware of its limitations and use it alongside other pain assessment methods for a comprehensive understanding of the patient’s experience.
McGill Pain Questionnaire (MPQ):

- A more complex questionnaire that measures the intensity, quality, and location of pain. It includes a list of words that patients can use to describe their pain.
The MPQ is a valuable tool for pain assessment in various situations, including:
- Chronic pain conditions: Chronic pain management requires understanding the different dimensions of pain patients experience. MPQ’s comprehensive assessment of sensory, affective, and evaluative qualities of pain helps tailor treatment plans.
- Acute pain: MPQ can be used to track the intensity and characteristics of acute pain after surgery or injuries, aiding in pain management decisions.
- Research: MPQ’s standardized format makes it suitable for research studies on pain mechanisms, treatment efficacy, and pain perception in various populations.
- Clinical trials: MPQ’s multidimensional approach can be used to evaluate the effectiveness of new pain medications or interventions in clinical trials.
- Communication: MPQ can facilitate communication between patients and healthcare providers by providing a structured way to describe pain experiences.
Ideal Patient for the MPQ
The MPQ is most suitable for patients who:
- Can understand and follow instructions: The questionnaire requires reading and comprehension, so cognitive limitations might make it challenging for some individuals.
- Can communicate effectively: Patients need to be able to describe their pain using the provided words or scales.
- Have a moderate level of literacy: Reading and writing skills are necessary to complete the questionnaire independently.
- Are motivated to participate: Patients need to be willing to invest time and effort in completing the questionnaire.
Pros and Cons of the MPQ
Pros:
- Comprehensive: Assesses multiple dimensions of pain, providing a richer understanding of the pain experience.
- Standardized: Scoring is standardized, making results comparable across different settings and studies.
- Valid and reliable: Well-validated and reliable tool with extensive research supporting its accuracy and consistency.
- Flexible: Can be used with various populations and pain types.
- Useful for communication: Provides a common language for describing pain, facilitating communication between patients and healthcare providers.
Cons:
- Time-consuming: Completing the questionnaire can take 5-10 minutes, which might be challenging for patients in acute pain.
- Complex: The wording of some descriptors might be difficult for some patients to understand.
- Cultural sensitivity: Some terms might not translate well across cultures, requiring adaptation for diverse populations.
- Limited for non-verbal patients: Patients with communication difficulties might not be able to use the MPQ effectively.
- Focus on self-report: Relies on the patient’s ability to accurately report their pain, which can be subjective.
Overall, the MPQ is a valuable tool for pain assessment when used in appropriate situations and with the right patient population. Its comprehensive nature and standardized format provide valuable information for pain management and research. However, its limitations, including time constraints, complexity, and reliance on self-report, should be considered when choosing the best pain assessment method for individual patients.
Defense and Veterans Pain Rating Scale (DVPRS):

- A self-reported pain scale developed for use with military personnel. It includes 10 pain descriptors and a 0-10 numeric rating scale.
When to Use:
- Military and veteran populations: The DVPRS was specifically designed for this population, considering their unique experiences and language.
- Chronic pain: It’s suitable for assessing chronic pain intensity and its impact on daily activities, sleep, mood, and stress.
- Acute pain: Can be used for acute pain, but other scales might be more efficient for rapid assessment.
- Limited communication abilities: The pictorial faces and color coding can be helpful for patients with communication difficulties.
Ideal Patient:
- Adults who understand the scale and can provide self-reported pain information.
- Patients familiar with military or veteran culture and language.
- Individuals experiencing chronic or acute pain, especially those with concerns about pain impacting daily life.
Pros:
- Multidimensional: Assesses pain intensity, functional impact, sleep, mood, and stress.
- Easy to use: Clear instructions, color coding, and facial expressions facilitate understanding.
- Reliable and valid: Research supports its accuracy in measuring pain in the target population.
- Standardized: Provides a common language for communication between patients and healthcare providers.
- Free and readily available: No licensing fees or restrictions on use.
Cons:
- Time-consuming: Takes longer to complete than some simpler pain scales.
- Not as widely used: May not be familiar to all healthcare providers.
- Limited validation: Requires further research on its effectiveness in specific populations and pain types.
- Potential for misinterpretation: Facial expressions and color coding might be interpreted differently by individuals.
- Limited customization: May not be suitable for all pain experiences or populations.
Overall, the DVPRS is a valuable tool for assessing pain in military and veteran populations, but its suitability depends on the specific patient and context. Healthcare providers should consider the pros and cons alongside other pain assessment tools to choose the best approach for each individual.
Adult Non-Verbal Pain Scale (ANVPA):

- Designed for patients with cognitive impairment or communication difficulties. It assesses four behavioral indicators: facial expression, vocalization, body movement, and resistance to care.
When to Use:
-
The ANVPA is best suited for adults who are unable to communicate verbally due to various reasons, such as:
- Intubation or mechanical ventilation
- Cognitive impairment or language difficulties
- Sedation or altered consciousness
- Unconsciousness
- Physical limitations preventing verbal communication
-
It can be used in various settings, including:
- Acute care hospitals (emergency department, intensive care unit, etc.)
- Long-term care facilities
- Hospice and palliative care settings
- Pain management clinics
- Dentistry and oral surgery settings
Ideal Patient:
- The ideal patient for the ANVPA is an adult who:
- Is at least 18 years old
- Has no visual or hearing impairments that would interfere with understanding the scale
- Has some level of cognitive awareness and ability to respond to physical prompts
- Is familiar with the concept of pain and can differentiate it from other sensations
Pros:
- Objective assessment: Provides an objective measure of pain based on observable behaviors, reducing reliance on subjective reports.
- Universally applicable: Can be used across diverse patient populations regardless of language, cultural background, or communication abilities.
- Increased pain detection: May help identify pain in patients who are unable to communicate it verbally, potentially leading to earlier intervention and improved pain management.
- Simple and quick: Can be administered quickly and easily with minimal training required for healthcare providers.
- Non-invasive: Does not require any physical contact with the patient, making it suitable for fragile or critically ill individuals.
Cons:
- Subjectivity in interpretation: Requires accurate interpretation of behaviors by healthcare providers, which can be subjective and prone to errors.
- Potential for misinterpretation: Certain behaviors might be misinterpreted as pain when they are due to other factors like discomfort, anxiety, or agitation.
- Limited sensitivity: May not be sensitive enough to detect subtle changes in pain in all patients.
- Patient cooperation: Requires some level of patient cooperation and awareness to respond to prompts, which may not be possible in all cases.
- Training and validation: Healthcare providers require training and validation in using the ANVPA to ensure accurate interpretation and reliable results.
Overall, the ANVPA is a valuable tool for pain assessment in non-verbal adults, but it should be used with caution and in conjunction with other clinical assessments to provide a comprehensive understanding of the patient’s pain experience.
-
Color Analog Pain Scale (CAPS):

- Uses a color gradient to represent pain intensity, with red being the most severe pain and blue being no pain. Patients select the color that best represents their pain.
When to Use CAPS:
- Children and adults with limited communication abilities: CAPS uses simple color gradients instead of numbers or words, making it suitable for individuals who have difficulty expressing their pain verbally.
- Patients with cognitive impairments: CAPS can be easier for individuals with dementia, intellectual disabilities, or language barriers to understand and use.
- Acute or chronic pain assessment: CAPS can be used to assess both short-term and long-term pain, allowing for monitoring of pain management interventions.
- Multi-cultural settings: The lack of language dependence makes CAPS a valuable tool in diverse healthcare settings.
Ideal Patient:
- Individuals with limited communication skills: Children under 3 years old, adults with speech impairments, or individuals with cognitive decline.
- Patients who struggle with numerical rating scales: Some individuals find numbers abstract or confusing, while colors can be more intuitive.
- Patients in pain management settings: CAPS can be used to track progress and adjust treatment plans.
Pros:
- Simple and easy to understand: The use of colors makes CAPS accessible to a wider range of patients.
- Non-verbal: No need for language skills, making it suitable for patients with communication difficulties.
- Sensitive to subtle changes in pain: The color gradient allows for finer distinctions in pain intensity compared to numeric scales.
- Culturally appropriate: Can be used across different cultures and languages.
- Quick and easy to administer: Can be completed in a short amount of time.
Cons:
- Subjectivity: Individual interpretations of colors can vary, leading to potential inconsistencies in pain assessment.
- Limited data on validity and reliability: CAPS is a relatively new tool, and further research is needed to confirm its effectiveness across different populations and pain types.
- May not be suitable for all patients: Some individuals with visual impairments or color blindness may find CAPS difficult to use.
- Lack of specific pain descriptors: Unlike some other scales, CAPS does not provide guidance on what each color represents in terms of pain intensity or quality.
Overall, the CAPS is a promising tool for pain assessment in a variety of settings. However, it is important to consider its limitations and choose the most appropriate pain scale based on the individual patient and the clinical context.
The best pain scale to use will depend on the individual patient and the situation. Some factors to consider include the patient’s age, cognitive ability, and level of pain. It is important to choose a scale that the patient can understand and use easily.
Resources on Pain Measurement Scales:
PDFs:
- Pain Assessment in Advanced Dementia Scale (PAINAD): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4443668/ This scale is specifically designed for assessing pain in people with dementia.
- McGill Pain Questionnaire (MPQ): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285427/ This is a more comprehensive questionnaire that assesses the sensory and affective dimensions of pain.
- Wong-Baker FACES Pain Rating Scale: https://www.physio-pedia.com/Faces_Pain_Scale_-_Revised This scale uses faces to represent different levels of pain, making it suitable for children and people with communication difficulties.
- Pain Assessment: How to Measure Pain Effectively: https://m.youtube.com/watch?v=Uo9zwOn-he8 This video from the American Physical Therapy Association provides a good overview of different pain assessment tools and how to use them effectively.
- Understanding Pain Scales: https://www.youtube.com/watch?v=jP1opUrxMR4 This video from the University of Michigan Health System explains how to use the Numerical Rating Scale and the Visual Analog Scale.
- Non-verbal Pain Assessment: https://www.youtube.com/watch?v=WdEpuwFD79s This video from the American Academy of Family Physicians demonstrates how to assess pain in people who are unable to communicate verbally.
- The National Pain Management Network: https://painmanagement.network/ This website provides information on pain management, including resources for healthcare professionals and patients.
- The National Institute of Nursing Research: https://www.ninr.nih.gov/ This institute funds research on pain management, including the development of new pain assessment tools.
- The National Center for Complementary and Integrative Health: https://www.nccih.nih.gov/ This center studies the use of complementary and integrative health practices for pain management.
- The American Pain Society: https://www.tpr.org/podcast/the-source/2023-01-31/american-pain-documentary This professional organization provides resources for healthcare professionals and patients on pain management, including information on pain assessment.
- The Joint Commission: https://www.jointcommission.org/ This organization sets standards for healthcare quality, including pain management.
I hope these resources help you learn more about pain measurement scales! Please let me know if you have any other questions.