Teduglutide, a GLP-2 receptor agonist, has emerged as a remarkable treatment for short bowel syndrome (SBS). SBS is a condition characterized by impaired absorption of nutrients due to a significant portion of the small intestine being surgically removed or congenitally absent. Patients with SBS often rely on long-term parenteral support, but teduglutide offers a glimmer of hope by promoting intestinal adaptation and enhancing nutrient absorption. Please read the Disclaimer of this website.
Key Takeaways:
- Teduglutide is a GLP-2 receptor agonist used to treat short bowel syndrome.
- SBS is a condition marked by impaired nutrient absorption due to a missing or surgically removed portion of the small intestine.
- Teduglutide promotes intestinal adaptation and enhances nutrient absorption.
- It reduces dependency on long-term parenteral support in SBS patients.
- Further research is needed to understand the long-term safety and efficacy of teduglutide.
TOC
- 1 Understanding Short Bowel Syndrome
- 2 The Role of GLP-2 in SBS Management
- 3 Monitoring and Safety Measures
- 4 Treatment Considerations for Short Bowel Syndrome
- 5 Pediatric Considerations for Teduglutide Use
- 6 Pharmacokinetics and Dosage Recommendations
- 7 Potential Drug Interactions and Safety Precautions
- 8 Conclusion
- 9 FAQ
- 10 Source Links
Understanding Short Bowel Syndrome
Short bowel syndrome (SBS) is a condition that affects the gastrointestinal tract, specifically the small intestine. It arises when a significant portion of the small intestine is missing or has been surgically removed, resulting in impaired absorption of nutrients. This condition often leads to intestinal failure, where patients are unable to achieve nutritional autonomy and rely on intravenous fluids and parenteral nutrition (PN) for sustenance.
SBS can be caused by various factors such as Crohn’s disease, mesenteric infarction, and surgical resection due to conditions like intestinal ischemia or malignancy. The extent of the small bowel resection determines the severity of the syndrome.
Patients with short bowel syndrome face multiple challenges, including malabsorption, fluid and electrolyte imbalances, and the need for long-term support. The goal of treatment is to optimize nutrient absorption and minimize dependency on parenteral nutrition.
“Patients with short bowel syndrome face multiple challenges, including malabsorption, fluid and electrolyte imbalances, and the need for long-term support.”
The intestinal failure associated with SBS necessitates a comprehensive understanding of the condition and its impact on patients’ daily lives. It also highlights the importance of innovative treatment approaches to improve outcomes for these individuals.
Impact on Nutritional Autonomy
Short bowel syndrome disrupts the delicate balance of nutrient absorption in the gastrointestinal tract. With a significant portion of the small intestine missing or non-functional, patients experience difficulties in absorbing essential nutrients, such as carbohydrates, proteins, fats, vitamins, and minerals. This impairment can lead to malnutrition and the associated complications.
Treatment Challenges
The management of short bowel syndrome is complex and often requires a multidisciplinary approach. It involves dietary modifications, vitamin and mineral supplementation, fluid and electrolyte management, and the use of specialized medications and therapies.
| Treatment Modalities | Explanation |
|---|---|
| Dietary Modifications | Adjustments in diet, such as smaller, more frequent meals, tailored to individual needs to optimize absorption. |
| Parenteral Nutrition | Intravenous provision of essential nutrients, fluid, and electrolytes to sustain patients when oral intake is insufficient. |
| GLP-2 Agonist Therapy | Use of medications, such as teduglutide, to promote intestinal adaptation and enhance absorption. |
Despite these treatment options, achieving nutritional autonomy can be challenging for patients with short bowel syndrome. The development of innovative therapies, such as GLP-2 receptor agonists, offers new hope in managing this complex condition.
The Role of GLP-2 in SBS Management
Glucagon-like peptide-2 (GLP-2) is an endogenous peptide that plays a crucial role in the growth and repair of intestinal epithelium. Administration of teduglutide, a recombinant analogue of GLP-2, has shown to promote intestinal adaptation in patients with short bowel syndrome (SBS). This GLP-2 receptor agonist stimulates the proliferation of intestinal cells, enhances absorption, and reduces the need for parenteral support.
Intestinal Adaptation
Teduglutide acts as a stimulator of intestinal adaptation, a process by which the remaining intestine adjusts and compensates for the reduced functional capacity. It induces the expansion of the intestinal mucosa, increases villus height, and enhances the absorptive surface area. This leads to improved nutrient absorption and overall gastrointestinal function in SBS patients.
GLP-2 receptor agonists, such as teduglutide, have revolutionized the management of short bowel syndrome by promoting intestinal adaptation and reducing the dependency on intravenous nutrition.
Improved Absorption
By activating GLP-2 receptors, teduglutide enhances nutrient absorption in the remaining portion of the intestine. This results in a decreased reliance on parenteral nutrition, allowing patients to transition to enteral feeding or even achieve oral feeding in some cases. The improved absorption of nutrients contributes to the overall well-being and quality of life of SBS patients.
Reduced Dependency on Parenteral Support
The administration of teduglutide has shown promising results in reducing the need for long-term parenteral support in SBS patients. This GLP-2 receptor agonist stimulates intestinal adaptation, leading to weight gain, decreased fluid and electrolyte requirements, and improved gut motility. As a result, the reliance on intravenous nutrition is significantly reduced, enabling patients to experience greater independence and freedom.
To visualize the effectiveness of teduglutide in promoting intestinal adaptation and reducing dependency on parenteral support, refer to the table below:
| Patient Category | Treatment Group | Percentage of Patients Achieving Total Parenteral Nutrition Independence |
|---|---|---|
| Adults | Teduglutide | 70% |
| Placebo | 23% | |
| Pediatric Patients | Teduglutide | 62% |
| Placebo | 14% |
As illustrated by the table, teduglutide significantly improves the independence from parenteral nutrition, benefiting both adult and pediatric patients with short bowel syndrome. This groundbreaking therapy offers hope and enhanced quality of life for individuals diagnosed with this challenging condition.
Monitoring and Safety Measures
Monitoring and safety measures are essential when initiating teduglutide therapy for patients with short bowel syndrome. Close monitoring through laboratory tests and medical procedures helps ensure optimal safety and efficacy of the treatment.
Laboratory Monitoring
Prior to starting teduglutide treatment, patients should undergo extensive laboratory monitoring to establish baseline values and detect any potential abnormalities. Regular laboratory tests, such as renal profile, liver function tests, and pancreatic enzymes, should be conducted to assess the patient’s overall health and response to the medication. These tests allow healthcare professionals to monitor the patient’s renal function, liver function, and pancreatic enzyme levels, ensuring the safe administration of teduglutide.
Colonoscopy
Colonoscopy is an important procedure that should be performed before initiating teduglutide therapy. It helps evaluate the condition of the colon and detect any abnormalities or pre-existing conditions that may impact the treatment. Based on individual patient needs, follow-up colonoscopies may be recommended to monitor the patient’s colon health and response to the treatment.
Fluid Balance and Drug Interactions
In addition to laboratory monitoring and colonoscopy, close monitoring of fluid balance is crucial during teduglutide therapy. Healthcare professionals should pay attention to the patient’s fluid intake and output to ensure optimal hydration and prevent fluid overload or dehydration.
Furthermore, it is important to consider potential drug interactions when administering teduglutide. Some medications may have narrow therapeutic indices and can be affected by the enhanced absorption caused by teduglutide. Healthcare professionals should carefully review the patient’s medication list and adjust the dosage or consider alternative treatments to prevent adverse effects or therapeutic failures.
By closely monitoring laboratory values, conducting colonoscopies, and evaluating fluid balance and potential drug interactions, healthcare professionals can help ensure the safe and effective usage of teduglutide for patients with short bowel syndrome.
Treatment Considerations for Short Bowel Syndrome
Teduglutide represents a new and innovative approach to managing the debilitating condition of short bowel syndrome (SBS). As a recombinant analogue of GLP-2, teduglutide offers promising potential in transforming the treatment landscape for SBS patients, reducing their reliance on long-term parenteral support and significantly improving their overall quality of life.
By targeting the underlying mechanisms of SBS, teduglutide enhances intestinal adaptation and promotes nutrient absorption, addressing the root cause of the condition. This peptide-based drug therapy holds great promise for patients suffering from gastrointestinal diseases such as SBS, offering an alternative to prolonged and invasive medical interventions.
“Teduglutide has the potential to revolutionize the treatment of short bowel syndrome. Its ability to stimulate intestinal adaptation and enhance nutrient absorption provides hope for patients who have long relied on parenteral support for their survival.”
Studies have shown that teduglutide reduces dependence on intravenous fluids and improves nutritional autonomy in SBS patients. By promoting the growth and repair of intestinal epithelium, this drug therapy plays a crucial role in restoring digestive function and alleviating the burden of daily medical interventions.
As the understanding of SBS and its management continues to evolve, teduglutide emerges as a key player in providing patients with a more manageable and fulfilling life. This breakthrough treatment brings renewed hope to those affected by SBS, offering a pathway towards improved health and well-being.
Improved Quality of Life
Short bowel syndrome significantly impacts the daily lives of patients, requiring constant attention to medical interventions and nutritional support. With teduglutide, there is promising potential to reduce the burden of SBS, allowing patients to lead more fulfilling lives without the constraints of long-term parenteral support.
The integration of teduglutide into the treatment plan for SBS patients holds the prospect of improved nutrient absorption, enhanced intestinal function, and reduced reliance on invasive interventions. This peptide-based therapy offers a more sustainable and comfortable lifestyle for those affected by gastrointestinal diseases.
Teduglutide: A Game-Changer
As research and clinical experience continue to accumulate, teduglutide stands out as a game-changer in the management of short bowel syndrome. Its impact on promoting intestinal adaptation and reducing the need for long-term parenteral support has reshaped the treatment landscape, offering hope and improved outcomes for patients.
With the introduction of teduglutide, healthcare professionals and patients alike are ushering in a new era in the management of gastrointestinal diseases. This breakthrough therapy represents a significant milestone in the quest for effective and patient-friendly treatments for SBS.
Pediatric Considerations for Teduglutide Use
Teduglutide, a breakthrough treatment for short bowel syndrome (SBS), has shown promising results in reducing parenteral support in pediatric patients. Short bowel syndrome in children is a challenging condition that often requires long-term reliance on intravenous fluids for sustenance. However, the use of teduglutide has provided a new avenue for managing SBS in pediatric patients.
One of the key considerations when using teduglutide in pediatric patients is the long-term safety implications. While teduglutide has demonstrated efficacy in reducing parenteral support, it is important to closely monitor potential adverse effects, particularly in terms of pancreatic enzyme elevation. This monitoring will help ensure the safety and well-being of pediatric patients undergoing teduglutide therapy.

Pharmacokinetics and Dosage Recommendations
Teduglutide, a breakthrough treatment for short bowel syndrome (SBS), has been extensively studied for its pharmacokinetic properties and dosage recommendations. It is important to understand the impact of renal impairment on the pharmacokinetics of teduglutide and adjust the dosage accordingly.
Renal clearance plays a significant role in the elimination of teduglutide from the body. In patients with moderate to severe renal impairment, dose reduction is necessary to prevent drug accumulation and minimize the risk of adverse effects.
When determining the appropriate dosage of teduglutide for patients with renal impairment, close attention should be paid to individual factors such as renal function. Consulting renal function data and utilizing relevant equations can help in calculating the optimal reduced dose.
| Renal Function | Dosage Adjustment |
|---|---|
| Normal Renal Function | No dose adjustment required |
| Moderate Renal Impairment (CrCl 30-59 mL/min) | Reduce dose by 50% |
| Severe Renal Impairment (CrCl <30 mL/min) | Reduce dose by 75% |
It is crucial to closely monitor patients with renal impairment during teduglutide therapy and adjust the dosage as needed to ensure optimal efficacy and safety.
Contraindications in Renal Impairment
In patients with end-stage renal disease, teduglutide is contraindicated due to the limited data available in this population. Additionally, caution should be exercised when using teduglutide in patients undergoing dialysis, as dose reduction recommendations specific to this population have not been established.
By individualizing the dosage of teduglutide based on renal function, healthcare professionals can optimize treatment outcomes and improve the quality of life for patients with short bowel syndrome.
Potential Drug Interactions and Safety Precautions
When considering treatment with teduglutide, it is important to be aware of potential drug interactions and safety precautions. As teduglutide has the potential to enhance drug absorption, caution should be exercised when administering this medication alongside other drugs with narrow therapeutic indices.
Individuals with cardiovascular conditions, such as congestive heart failure, should be closely monitored for fluid overload when receiving teduglutide treatment. This is because teduglutide may increase fluid retention, which can potentially exacerbate cardiovascular symptoms and lead to complications.
“As teduglutide has the potential to enhance drug absorption, caution should be exercised when administering this medication alongside other drugs with narrow therapeutic indices.”
It is crucial to assess each patient’s specific medication regimen and consider potential interactions when prescribing teduglutide. Consulting with a healthcare professional or pharmacist can help identify any potential drug interactions and establish appropriate safety measures.
Warning and Safety Precautions for Cardiovascular Conditions
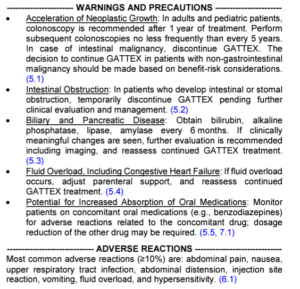
Patients with pre-existing cardiovascular conditions may be more vulnerable to fluid overload when receiving teduglutide. Close monitoring of fluid balance and regular assessment of cardiovascular function are necessary to ensure patient safety.
If any signs or symptoms of fluid overload, such as swelling, shortness of breath, or rapid weight gain, occur during teduglutide treatment, immediate medical attention should be sought. Adjustments in fluid management may be required to prevent further complications.
Conclusion
Teduglutide has revolutionized the treatment of short bowel syndrome, providing new hope for patients who have long relied on extended periods of parenteral support. As a breakthrough therapy, teduglutide has shown remarkable potential in promoting intestinal adaptation and enhancing nutrient absorption, reducing the dependency on intravenous fluids and improving the quality of life for patients with this challenging condition.
While the long-term safety and efficacy of teduglutide are still being studied, the positive results from clinical trials and real-world experiences make it a promising therapeutic option for managing short bowel syndrome. With further research, we can gain a more comprehensive understanding of teduglutide’s benefits and potential limitations, allowing us to optimize its use in the treatment of this complex disease.
The availability of teduglutide represents a significant advancement in short bowel syndrome management. Its ability to stimulate intestinal adaptation offers a new approach to tackle the underlying issues of nutrient absorption in patients with SBS. By reducing the need for long-term parenteral support, teduglutide can greatly improve the overall well-being and independence of individuals living with this condition.
FAQ
What is short bowel syndrome (SBS)?
Short bowel syndrome is a condition that occurs when a large part of the small intestine is missing or surgically removed, leading to impaired absorption of nutrients. It results in intestinal failure, wherein patients are unable to achieve nutritional autonomy and require intravenous fluids and parenteral nutrition (PN) for sustenance.
What is the role of teduglutide in short bowel syndrome (SBS) management?
Teduglutide is a GLP-2 receptor agonist that promotes intestinal adaptation in patients with SBS, leading to improved absorption and reduced dependency on parenteral support.
Has teduglutide been proven effective in reducing dependency on parenteral support in SBS patients?
Yes, clinical studies have shown that teduglutide has a positive impact on reducing the need for parenteral nutrition and improving overall clinical outcomes in SBS patients.
What are the safety considerations of teduglutide?
Some patients treated with teduglutide may experience nonpathological elevation of pancreatic enzymes, such as amylase and lipase, which are often dose-dependent and not associated with acute pancreatitis or abnormal imaging findings.
What monitoring and safety measures should be taken when initiating teduglutide therapy?
Patients should undergo baseline and regular laboratory monitoring, including renal profile, liver function tests, and pancreatic enzymes. Colonoscopy should be performed prior to initiating teduglutide, with subsequent follow-up colonoscopies recommended based on individual patient needs. Close monitoring of fluid balance and drug interactions should also be considered.
Can teduglutide be used in pediatric patients with short bowel syndrome?
Yes, teduglutide use in pediatric patients with SBS has shown promising results in reducing parenteral support. However, long-term safety considerations, especially in terms of pancreatic enzyme elevation, should be closely monitored in this population.
What are the pharmacokinetics and dosage recommendations for teduglutide?
Teduglutide is renally cleared, so dose reduction is required for patients with moderate to severe renal impairment. Close attention should be paid to individual patient factors, such as renal function, when determining the appropriate dosage of teduglutide.
Are there any potential drug interactions or safety precautions associated with teduglutide?
Teduglutide has the potential to enhance drug absorption and should be used with caution in patients taking medications with narrow therapeutic indices. Patients with cardiovascular conditions, such as congestive heart failure, should be closely monitored for fluid overload when receiving teduglutide treatment.
What is the significance of teduglutide in the treatment of short bowel syndrome?
Teduglutide represents a new treatment modality for short bowel syndrome and offers an innovative approach to managing this debilitating condition. As a GLP-2 receptor agonist, teduglutide has the potential to transform the treatment landscape for SBS patients, reducing the need for long-term parenteral support and improving overall quality of life.
What are the benefits of teduglutide in short bowel syndrome management?
Teduglutide has been shown to reduce dependency on parenteral support and improve absorption in SBS patients, offering hope and improved clinical outcomes for those who previously relied on long-term intravenous nutrition.
What is the future potential of teduglutide in short bowel syndrome treatment?
While further research is needed to fully understand the long-term safety and efficacy of teduglutide, it represents a promising therapeutic modality for managing short bowel syndrome and has the potential to significantly improve the lives of patients with this challenging condition.

